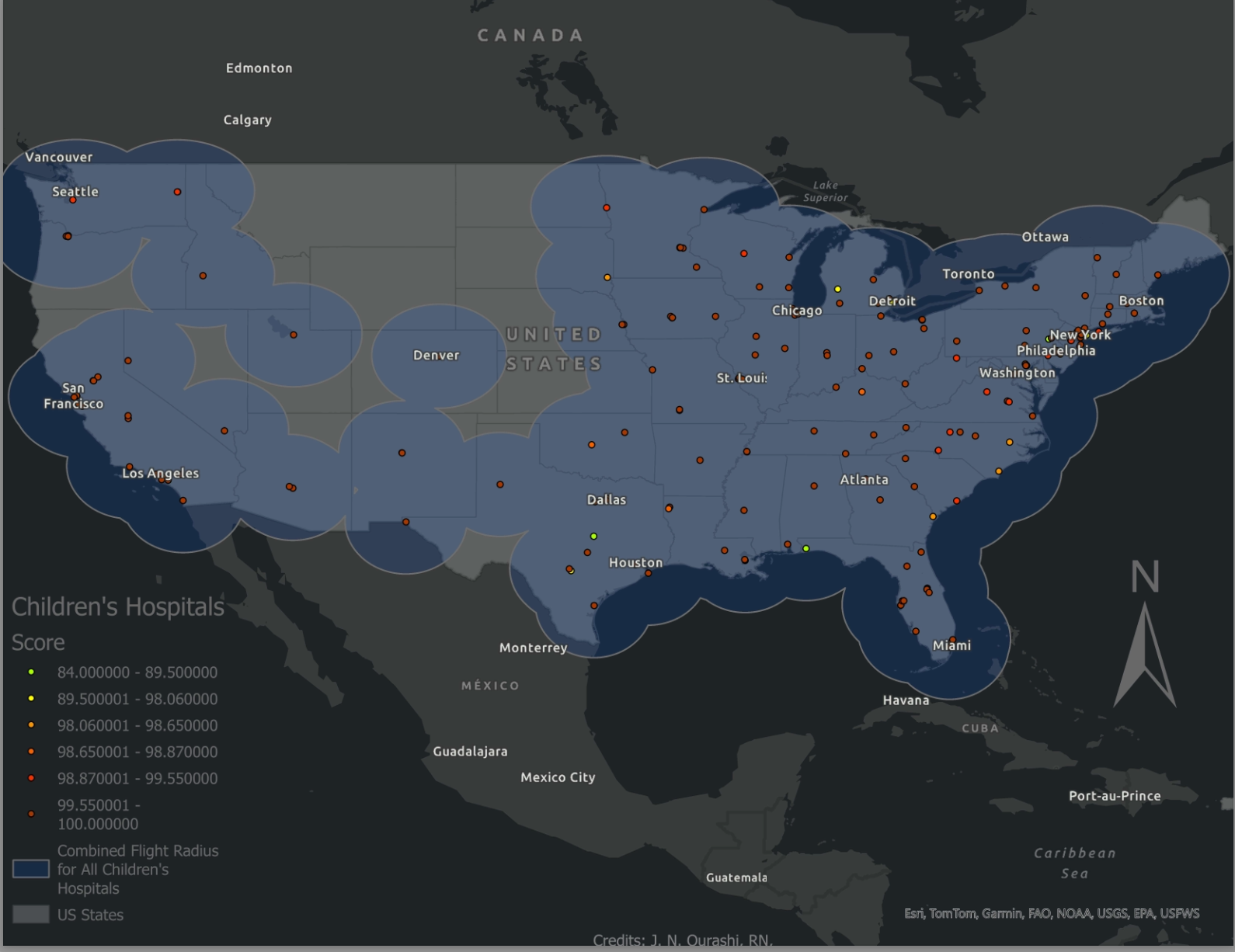
When the unimaginable happens, your child’s access to care shouldn’t be delayed by INVISIBLE lines
The Interstate Transport Project
Interfacility transport is an essential part of the modern healthcare system. It connects isolated, less resourced communities with tertiary and quaternary care centers – thus improving access to care, especially when patients are in critical condition and time is life. This is particularly true in the case of paediatric patients who require care by specialty physicians and surgeons and in times of natural or man-made disaster.
What is interfacility medical transport?
In the United States, our healthcare system is based around hospital systems. Most communities have access to some kind of hospital facility or a regional center which cares for several communities in the vicinity. For advanced medical needs patients must be seen at a tertiary care center, typically a level 1 trauma center that can manage specialty surgical needs.
With so many fewer children’s hospitals, this is especially true for paediatric patients. Connecting children to these specialty centers becomes increasingly difficulty with the severity of the child’s illness or injury and the distance they are from pediatric specialists.
If a patient is stable, the child’s parents may arrange for transportation via private vehicle, buses, trains, or commercial airliners. If the patient is too sick to be out of a physician’s care, medical transport is used to connect children with critical resources.
This is accomplished via surface transport, like ambulances, and air transport which includes fixed-wing transport, like leer jets and commercial airliners with medical crew, and rotor- wing transport on helicopters. What makes medical transport special is the crew of expert clinicians that travel with the patient providing medical care under the direction of a physician.
What’s the problem?
Basically, it is crossing state lines. Teams are licensed at the state level. Unlike driver’s licenses which are recognized between states, clinicians are not always allowed to practice at the same level after crossing the border.
When states relegate providers to lower levels, it disqualifies a competent crew from performing the transport. This can delay care and restricts timely access to treatment.
36.6% of the total US population lives in a community that borders or crosses state lines.
94.5% of children’s hospitals transport radii include neighbouring states
Why can’t we just fix it?
The biggest roadblock to change is lack of problem recognition. Inter-facility transport is a niche field. And, on average, across the nation, interstate transport doesn’t happen all that often. But it is a major problem for paediatric patients. Transport of adult patients experiences similar complexities during times of disaster like the COVID-19 pandemic. The purpose of this study is to bring awareness of the issue by providing supporting evidence.
Why This Matters
Hear a first hand account about how delays in pediatric interstate transport cost a young boy more than time — and why we have to fix this.
Creating change.
-

Research
Good policy starts with the facts. Since 2018 we have been collecting data on transport activities and EMS law across the country. Learn more about the regulations in your state and its neighbors.
-
Solutions
It is one thing to identify a problem, but quite another to solve it. Learn more about the currently patches to the system and our ideas to create an equitable solution nationwide.
-

Policy
Legislation is our goal. We believe a federal solution to our disjointed system will decrease wait times and improve health outcomes. Learn more about our proposed changes and how you can support.
A word from the Frontline
Health care providers often feel frustrated when their hands are tied by regulations that prevent a willing and able team from providing needed care. This is Nelson Carver, NRP, FP-C. He is a flight medic and father and wants to tell you his perspective.